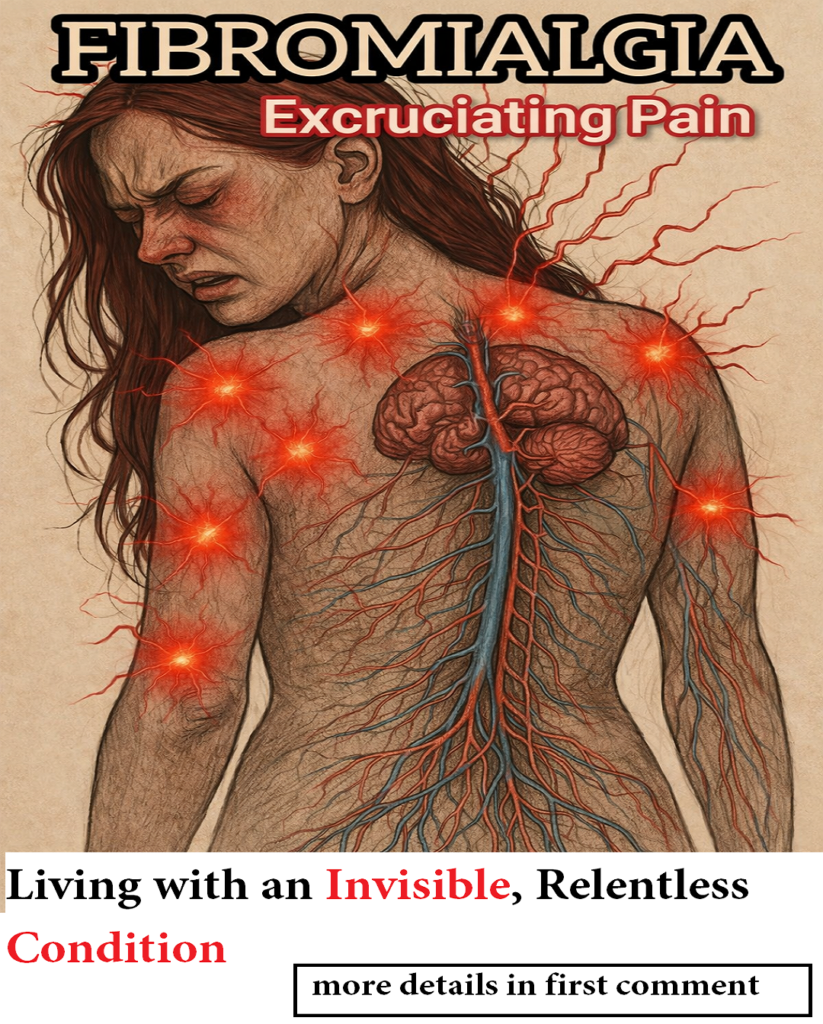
Fibromyalgia is often described as a condition of widespread muscle pain and fatigue, but for many people living with it, the suffering goes far deeper than aching joints or tender points. One of the most misunderstood and distressing symptoms is skin sensitivity and chronic itching—a sensation that feels intense, relentless, and very real, even when the skin looks completely normal.
For those experiencing it, fibromyalgia can make the skin feel as though it is burning, crawling, stinging, or itching from the inside out. Clothing can feel unbearable. A light touch may cause discomfort. Even air moving across the skin can trigger irritation. Yet, because there are often no visible rashes, redness, or lesions, this symptom is frequently dismissed or misdiagnosed as anxiety, allergies, or imagination.
The truth is clear: in fibromyalgia, even the skin can hurt. And science increasingly supports what patients have been saying for years.
Fibromyalgia and the Nervous System: More Than Muscle Pain
To understand why itching and skin sensitivity occur in fibromyalgia, it is essential to look at the condition through a neurological lens.
Fibromyalgia is now widely recognized as a central nervous system disorder, not simply a musculoskeletal condition. The defining feature of fibromyalgia is central sensitization, a state in which the brain and spinal cord become overly responsive to sensory input.
In a healthy nervous system, sensations like light touch, temperature changes, or fabric against the skin are processed as neutral or mild. In fibromyalgia, however, the nervous system amplifies these signals, interpreting them as painful, irritating, or overwhelming.
This hypersensitivity does not stop at pain. It also affects itch perception, which is processed through many of the same neural pathways as pain. As a result, sensations that would not normally provoke itching—such as seams in clothing, dry air, or gentle pressure—can become intensely uncomfortable.
This neurological overreaction explains why fibromyalgia symptoms can feel unpredictable, disproportionate, and difficult to explain to others.
Why Itching in Fibromyalgia Often Has No Visible Cause
One of the most frustrating aspects of fibromyalgia-related itching is that it often occurs without any visible skin changes.
There may be:
-
No rash
-
No redness
-
No hives
-
No swelling
And yet, the itching can feel severe, persistent, and uncontrollable.
This happens because the problem does not originate in the skin itself, but in the sensory nerves beneath the skin and the way the brain interprets their signals. These nerves become hypersensitive and send exaggerated messages to the brain, which then registers the sensation as itching, burning, tingling, or crawling.
Because there is no obvious dermatological explanation, many people are misdiagnosed with allergies, eczema, or psychosomatic conditions. Others are told that stress is the only cause. While stress can worsen symptoms, it is not the root cause.
The itching in fibromyalgia is neurological, not imaginary.
The Role of Neurochemical Imbalances in Skin Sensations
Fibromyalgia is associated with significant neurochemical imbalances, particularly involving substances that regulate pain, mood, sleep, and sensory perception.
Two of the most important are:
Serotonin
Serotonin helps regulate pain thresholds, sleep cycles, mood, and sensory processing. People with fibromyalgia often have lower levels of serotonin, which can increase sensitivity to pain and itching while also contributing to anxiety, depression, and sleep disturbances.
Substance P
Substance P is a neurotransmitter involved in transmitting pain and sensory signals. Studies show that individuals with fibromyalgia have elevated levels of substance P in their cerebrospinal fluid. High levels of this chemical intensify the perception of pain and itch, making even mild stimuli feel severe.
Together, these imbalances help explain why fibromyalgia itching is often described as:
-
Burning or stinging
-
Deep and internal
-
Worse at night
-
Accompanied by tingling or pins-and-needles sensations
This neurochemical dysregulation also explains why antihistamines often fail to relieve the itching—because histamine is not the primary driver.
Triggers That Make Skin Sensitivity and Itching Worse
Although fibromyalgia itching can occur spontaneously, certain factors are known to intensify skin sensitivity and provoke flare-ups.
Stress and Emotional Overload
Stress directly affects the nervous system. In fibromyalgia, emotional stress can lower the threshold for sensory tolerance, making itching and discomfort more intense and harder to control.
Extreme Fatigue
When the body is exhausted, the nervous system becomes less capable of regulating sensory input. This is why itching often worsens after physically or mentally demanding days.
Poor Sleep
Sleep disturbances are a core symptom of fibromyalgia. Lack of restorative sleep increases central sensitization, which in turn amplifies itching, burning, and pain—especially during the night.
Temperature Changes
Cold air, heat, humidity, or sudden temperature shifts can overstimulate sensitive skin nerves. Many people with fibromyalgia report worse itching in winter due to dry air, or in summer due to heat and sweating.
Dry Skin
Fibromyalgia is sometimes associated with autonomic nervous system dysfunction, which can reduce normal skin hydration. Dry skin alone does not cause fibromyalgia itching, but it can intensify the sensation and increase discomfort.
When Itching Becomes a Nighttime Battle
For many people with fibromyalgia, itching becomes especially severe at night. This is not a coincidence.
At night:
-
External distractions decrease
-
The nervous system becomes more aware of internal sensations
-
Body temperature regulation changes
-
Fatigue peaks
As a result, itching, burning, and crawling sensations can feel more intense, interfering with already fragile sleep patterns. Scratching may provide brief relief but often worsens the problem by irritating the skin and reinforcing the sensory feedback loop.
This cycle—itching, scratching, poor sleep, increased sensitization—can become exhausting both physically and emotionally.
Managing Fibromyalgia-Related Skin Sensitivity and Itching
While there is no single cure for fibromyalgia itching, a comprehensive, gentle approach can significantly reduce its impact.
Prioritize Skin Hydration
Using fragrance-free, hypoallergenic moisturizers helps protect the skin barrier and reduce dryness-related irritation. Hydrated skin is less likely to trigger hypersensitive nerves.
Choose Soft, Breathable Clothing
Loose-fitting clothes made from cotton, bamboo, or silk are often better tolerated. Avoid rough fabrics, tight seams, tags, and synthetic materials that can overstimulate the skin.
Reduce Nervous System Overload
Stress-management techniques such as deep breathing, meditation, pacing, and gentle movement help calm the nervous system and reduce sensory amplification.
Improve Sleep Quality
Consistent sleep routines, reduced screen exposure before bed, and treatment of sleep disorders can lower central sensitization and decrease nighttime itching.
Treat Fibromyalgia as a Whole
Because itching is part of the neurological process, managing overall fibromyalgia symptoms—pain, fatigue, mood, and sleep—often leads to improvements in skin sensitivity as well.
It is important to note that excessive scratching can cause secondary skin injuries. The goal is not just to soothe the skin, but to address the neurological source of the symptom.
The Emotional Impact of Invisible Symptoms
Perhaps one of the hardest aspects of fibromyalgia-related itching is that it is invisible. Friends, family, and even healthcare providers may struggle to understand how something unseen can be so distressing.
Being told “there’s nothing wrong with your skin” can feel invalidating when your body is clearly signaling discomfort. Over time, this dismissal can lead to frustration, self-doubt, and emotional exhaustion.
Acknowledging that the itch is real—and rooted in neurological changes—is an essential step toward compassion, validation, and proper care.
Fibromyalgia: When Even the Skin Hurts
Fibromyalgia is not limited to muscles and joints. It affects the entire sensory system, including the skin. The itching may be invisible, but it is persistent. It may not leave marks, but it leaves an impact.
Understanding that fibromyalgia-related skin sensitivity is a neurological symptom, not an allergy or imagination, helps shift the conversation from disbelief to support.
For those living with fibromyalgia, the message is simple but powerful:
Your experience is real.
Your symptoms are valid.
And yes—even the skin can hurt.