Hip pain can be frustrating, exhausting, and life-altering—especially when it becomes chronic. Two conditions frequently associated with persistent hip discomfort are trochanteric bursitis and fibromyalgia. While each can exist independently, many individuals experience both simultaneously, resulting in intensified pain, disturbed sleep, and reduced quality of life. Understanding how these conditions interact is essential for proper management and relief.
In this article, we explore the relationship between trochanteric bursitis and fibromyalgia, common symptoms, causes, diagnosis, and effective treatment strategies to help you regain control over your daily life.
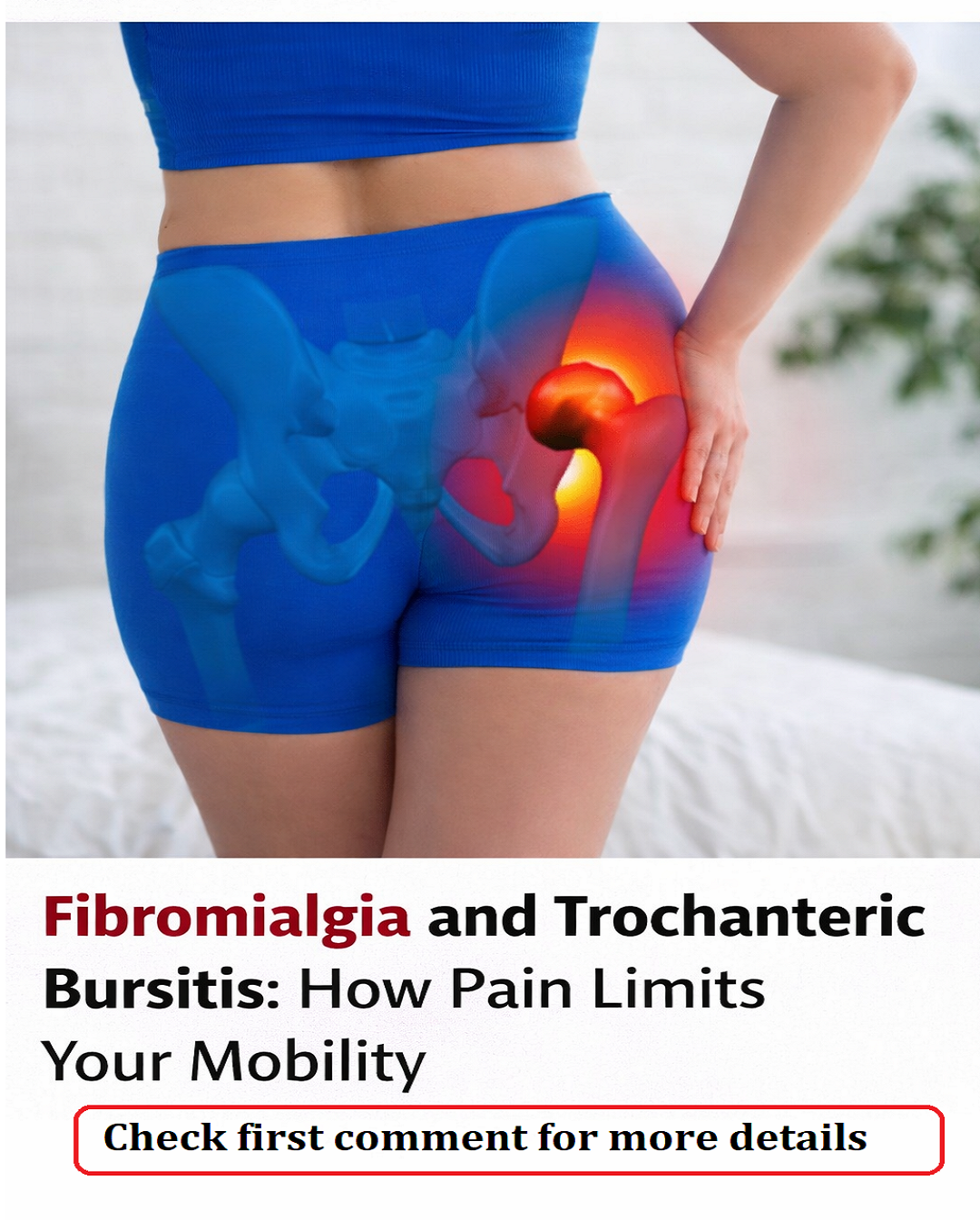
What Is Trochanteric Bursitis?
Trochanteric bursitis is a common cause of outer hip pain. It occurs when the trochanteric bursa—a small fluid-filled sac located on the outer side of the hip—becomes inflamed. This bursa acts as a cushion, reducing friction between the hip bone (femur), muscles, and tendons during movement.
When inflamed, the bursa loses its protective function, causing pain and tenderness around the hip area.
Common Symptoms of Trochanteric Bursitis
People suffering from trochanteric bursitis often experience:
-
Sharp or aching pain on the outside of the hip
-
Pain that worsens when walking, climbing stairs, or standing for long periods
-
Discomfort when lying on the affected side
-
Tenderness when pressing the outer hip
-
Pain radiating down the outer thigh or buttock
-
Stiffness after inactivity
This pain may start mildly but can become persistent if left untreated.
Understanding Fibromyalgia
Fibromyalgia is a chronic pain disorder that affects how the brain and nervous system process pain signals. People with fibromyalgia often experience widespread body pain, fatigue, sleep disturbances, and increased sensitivity to pressure.
Unlike trochanteric bursitis, fibromyalgia is not caused by localized inflammation. Instead, it involves central sensitization, meaning the nervous system amplifies pain signals—even when physical injury or inflammation is minimal.
Common Symptoms of Fibromyalgia
-
Widespread muscle pain and tenderness
-
Chronic fatigue
-
Sleep problems (non-restorative sleep)
-
Brain fog and difficulty concentrating
-
Muscle stiffness and weakness
-
Heightened pain sensitivity
-
Headaches and mood disturbances
Fibromyalgia affects the entire body, but it can also intensify pain from other conditions, including bursitis.
How Trochanteric Bursitis and Fibromyalgia Are Connected
Trochanteric bursitis and fibromyalgia often coexist, creating a complex pain pattern that is both localized and widespread. While bursitis causes inflammation in the hip region, fibromyalgia amplifies the perception of pain, making symptoms more severe and persistent.
Why the Pain Feels Worse Together
Several factors contribute to increased discomfort when both conditions are present:
1. Pain Amplification
Fibromyalgia causes the nervous system to remain in a heightened state, amplifying even mild inflammation from bursitis.
2. Altered Gait and Movement
Muscle stiffness, weakness, and fatigue in fibromyalgia can change how a person walks, placing extra stress on the hip and increasing the risk of bursitis.
3. Muscle Overload
Certain muscle groups compensate for weakness, causing repetitive strain and friction around the trochanteric bursa.
4. Chronic Inflammation Sensitivity
Even minimal swelling in the hip can feel extremely painful due to fibromyalgia-related hypersensitivity.
Symptoms When Both Conditions Occur Together
When trochanteric bursitis and fibromyalgia coexist, symptoms often become more widespread and harder to manage.
Common combined symptoms include:
-
Persistent outer hip pain
-
Pain spreading to the thigh, buttock, or lower back
-
Difficulty sleeping due to nighttime hip discomfort
-
Tenderness around the hip and surrounding muscles
-
Fatigue and reduced mobility
-
Pain mistaken for sciatica
-
Increased stiffness and weakness
Nighttime pain is particularly common. Many individuals cannot lie on the affected side, which further disrupts sleep—a major concern in fibromyalgia management.
Causes and Risk Factors
Several factors increase the likelihood of developing trochanteric bursitis alongside fibromyalgia.
Mechanical Causes
-
Repetitive hip movements
-
Poor posture
-
Leg length differences
-
Muscle imbalance
-
Weak hip stabilizing muscles
Lifestyle and Health Factors
-
Sedentary lifestyle
-
Obesity or excess body weight
-
Previous hip injuries
-
Overuse from physical activity
-
Chronic inflammation
Fibromyalgia contributes indirectly by increasing muscle tension, fatigue, and pain sensitivity, which may lead to abnormal movement patterns and additional stress on the hip.
How Pain Radiates and Mimics Other Conditions
One challenge in diagnosis is that pain from trochanteric bursitis can radiate beyond the hip, sometimes resembling other conditions.
Pain may spread to:
-
Outer thigh
-
Buttock
-
Lower back
-
Pelvic region
Because of this radiation, trochanteric bursitis is often confused with sciatica, hip arthritis, or lumbar spine problems. Accurate diagnosis is crucial to ensure proper treatment.
Diagnosis: Identifying the Root Cause
A healthcare professional typically diagnoses trochanteric bursitis through:
-
Physical examination
-
Tenderness over the outer hip
-
Pain during hip movement
-
Medical history review
In some cases, imaging tests such as ultrasound or MRI may be used to confirm inflammation or rule out other conditions.
Fibromyalgia is diagnosed based on:
-
Widespread pain lasting more than three months
-
Tender points throughout the body
-
Fatigue and sleep disturbances
-
Exclusion of other disorders
Because symptoms overlap, doctors must evaluate both local inflammation and central nervous system sensitivity.
Treatment Options for Trochanteric Bursitis with Fibromyalgia
Managing both conditions requires a multidimensional approach targeting inflammation, pain processing, and mechanical stress.
1. Physical Therapy
Physical therapy is one of the most effective treatments. It helps:
-
Strengthen hip and core muscles
-
Improve posture and walking pattern
-
Reduce pressure on the hip bursa
-
Increase flexibility
Stretching the iliotibial band and strengthening hip stabilizers can significantly reduce pain.
2. Pain Management
Pain relief strategies may include:
-
Anti-inflammatory medications
-
Ice therapy for localized swelling
-
Heat therapy for muscle stiffness
-
Topical pain relievers
For fibromyalgia-related pain, doctors may prescribe medications that regulate pain signals in the nervous system.
3. Lifestyle Adjustments
Simple lifestyle changes can reduce stress on the hip and improve overall symptoms:
-
Avoid lying on the affected side
-
Use supportive pillows while sleeping
-
Maintain healthy body weight
-
Avoid prolonged standing or sitting
-
Wear supportive footwear
4. Exercise and Movement
Gentle, low-impact exercise is essential for both bursitis and fibromyalgia.
Recommended activities include:
-
Walking
-
Swimming
-
Yoga
-
Stretching routines
Regular movement improves circulation, reduces stiffness, and enhances muscle balance.
5. Sleep Improvement
Since both conditions disrupt sleep, improving sleep quality is critical.
Tips include:
-
Maintain consistent sleep schedule
-
Use supportive mattress and pillows
-
Avoid caffeine before bedtime
-
Practice relaxation techniques
Better sleep reduces pain sensitivity and improves recovery.
6. Stress and Nervous System Regulation
Fibromyalgia is closely linked to nervous system overstimulation. Stress reduction can significantly improve symptoms.
Helpful methods include:
-
Mindfulness and meditation
-
Deep breathing exercises
-
Gentle stretching
-
Cognitive behavioral therapy
These approaches calm the nervous system and reduce pain amplification.
Long-Term Management and Outlook
While neither fibromyalgia nor trochanteric bursitis has a quick cure, both can be effectively managed. Early recognition of their coexistence allows for better care and symptom control.
Long-term management focuses on:
-
Controlling inflammation
-
Improving muscle balance
-
Regulating pain processing
-
Enhancing mobility and strength
-
Preventing flare-ups
Most individuals experience improvement with consistent treatment and lifestyle modifications.
When to Seek Medical Help
Consult a healthcare professional if you experience:
-
Persistent hip pain lasting more than a few weeks
-
Pain interfering with sleep or mobility
-
Widespread body pain and fatigue
-
Difficulty walking or climbing stairs
-
Pain radiating to lower back or leg
Early diagnosis prevents chronic worsening and helps tailor treatment to your needs.
Final Thoughts
The relationship between trochanteric bursitis and fibromyalgia highlights the complexity of chronic pain. It is not always caused by a single source but often results from a combination of local inflammation, mechanical stress, and nervous system sensitivity.
Recognizing this connection empowers patients and healthcare providers to adopt a comprehensive treatment approach—one that respects the body’s limitations while addressing the underlying causes of pain.
With proper care, lifestyle adjustments, and consistent management, individuals living with both conditions can achieve meaningful relief, improved sleep, and a better quality of life.