Chest pain is one of the most alarming symptoms a person can experience. When it happens repeatedly, without clear test results or explanations, it can become emotionally exhausting. For people living with fibromyalgia, chest pain is not uncommon, yet it is frequently misunderstood, misdiagnosed, or dismissed. One of the most common sources of confusion is the overlap between fibromyalgia chest pain and costochondritis, a condition involving inflammation of the rib cartilage.
Although the pain may feel identical, the underlying causes are often very different. Understanding this distinction is essential—not only for accurate diagnosis, but also for emotional reassurance, effective treatment, and long-term quality of life.
This article explores the complex relationship between fibromyalgia and costochondritis, why chest pain occurs even without inflammation, and how recognizing the difference can reduce fear, frustration, and unnecessary medical interventions.
What Is Fibromyalgia and How Does It Affect Pain Perception?
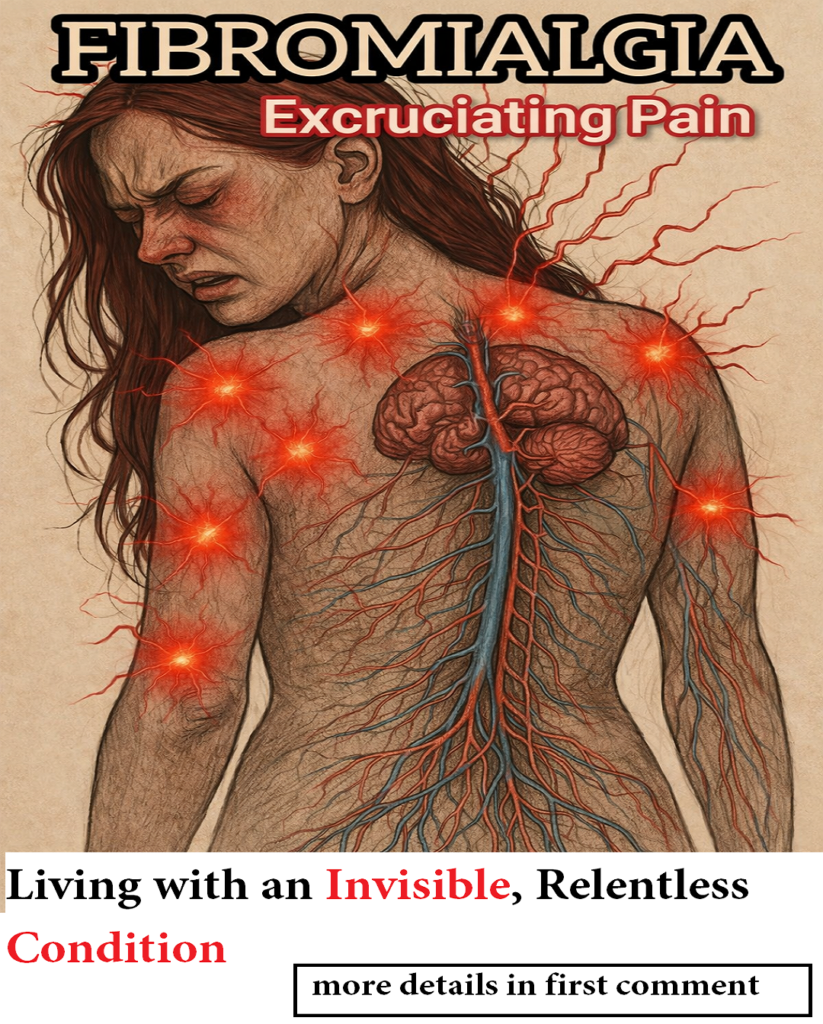
Fibromyalgia is a chronic pain condition characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and heightened sensitivity to physical stimuli. Unlike inflammatory or degenerative diseases, fibromyalgia does not cause visible damage to joints, muscles, or tissues. Instead, it affects how the nervous system processes pain.
In people with fibromyalgia, the brain and spinal cord amplify pain signals. Sensations that would normally be mild—or not painful at all—are perceived as intense, persistent discomfort. This phenomenon is known as central sensitization, and it plays a key role in why fibromyalgia pain can appear in unexpected places, including the chest wall.
Importantly, fibromyalgia pain is real and disabling, even when imaging scans, blood tests, and physical exams appear normal. The absence of visible inflammation does not mean the absence of suffering.
What Is Costochondritis? Understanding Inflammatory Chest Wall Pain
Costochondritis is a condition involving inflammation of the cartilage that connects the ribs to the sternum (breastbone). This inflammation can cause sharp, aching, or pressure-like pain in the chest, often worsening with movement, deep breathing, coughing, or physical activity.
Typical features of costochondritis include:
-
Localized pain along the rib joints
-
Tenderness when pressing on specific points near the sternum
-
Pain that increases with chest movement or exertion
-
Usually normal heart and lung tests
Costochondritis is often temporary and may be triggered by physical strain, injury, repetitive movements, respiratory infections, or prolonged coughing. In many cases, it improves with rest and anti-inflammatory treatment.
However, when chest pain persists for months, returns repeatedly, or spreads beyond a localized area, the explanation may not be purely inflammatory.
Why Fibromyalgia Chest Pain Feels Like Costochondritis
One of the most challenging aspects of fibromyalgia is that it can mimic other conditions almost perfectly. Chest pain related to fibromyalgia often feels identical to costochondritis—tight, stabbing, burning, or crushing—especially when breathing deeply or changing position.
The key difference lies beneath the surface.
In fibromyalgia, chest pain often occurs without any detectable inflammation. Instead, the nerves in the rib cage and sternum become hypersensitive. Normal chest wall movements—such as breathing, turning in bed, stretching, or even gentle touch—can be interpreted by the nervous system as severe pain.
Common features of fibromyalgia-related chest pain include:
-
Pain that moves or changes location
-
Widespread tenderness rather than one inflamed spot
-
Discomfort triggered by light pressure or clothing
-
Pain that fluctuates over days or weeks
-
Normal imaging and blood tests
Because the rib cage moves constantly with breathing, this area is particularly vulnerable to pain amplification in fibromyalgia. Even without injury or inflammation, the nervous system reacts as if the area is under threat.
Can Fibromyalgia and Costochondritis Occur Together?
Yes—fibromyalgia and costochondritis can coexist. Having fibromyalgia does not protect someone from developing true inflammatory conditions, and a person with fibromyalgia may experience costochondritis due to physical strain, illness, or injury.
However, the problem arises when all chest pain in fibromyalgia is automatically labeled as costochondritis, especially when no signs of inflammation are present. This can lead to:
-
Repeated use of anti-inflammatory medications that provide little relief
-
Frustration when symptoms persist despite “treatment”
-
Delayed recognition of nervous system involvement
-
Increased anxiety and medical uncertainty
In many cases, the diagnosis of costochondritis is made based solely on pain location, without considering central sensitization. As a result, people may be told they have recurring inflammation when the real issue is a pain-processing disorder.
Understanding whether pain is inflammatory, neurological, or both is crucial for choosing the right management approach.
Why Chest Pain in Fibromyalgia Causes So Much Fear and Anxiety
Chest pain carries a unique emotional weight. Because of its proximity to the heart, it often triggers fear of heart attack, lung disease, or other life-threatening conditions. Many people with fibromyalgia describe making repeated emergency room visits, only to be told that “everything looks normal.”
While ruling out cardiac causes is essential, the emotional impact of persistent chest pain should not be underestimated. Even after serious conditions are excluded, the pain remains—real, intense, and limiting.
This cycle can lead to:
-
Health anxiety and hypervigilance
-
Fear of movement or exercise
-
Sleep disturbances
-
Increased pain sensitivity due to stress
-
Feelings of not being believed or understood
Stress and anxiety further activate the nervous system, which can worsen fibromyalgia symptoms. This creates a feedback loop where pain increases fear, and fear increases pain.
Validation and understanding are therefore not just emotionally supportive—they are part of effective symptom management.
How to Tell the Difference Between Costochondritis and Fibromyalgia Chest Pain
Distinguishing between costochondritis and fibromyalgia-related chest pain is not always straightforward, but certain patterns can help guide understanding.
Costochondritis is more likely when:
-
Pain is sharply localized to one or two rib joints
-
There is clear tenderness at specific cartilage points
-
Pain improves with anti-inflammatory treatment
-
Symptoms follow physical strain or illness
Fibromyalgia chest pain is more likely when:
-
Pain is widespread or migratory
-
Multiple tender areas are present elsewhere in the body
-
Tests repeatedly show no inflammation
-
Pain fluctuates without clear physical triggers
-
Other fibromyalgia symptoms are active
Ultimately, diagnosis should be based on the overall clinical picture, not just pain location.
Why Standard Tests Are Often Normal in Fibromyalgia Chest Pain
One of the most frustrating aspects of fibromyalgia is that standard diagnostic tests rarely show abnormalities. X-rays, MRIs, blood tests, and inflammatory markers are typically normal—even when pain is severe.
This does not mean the pain is imagined. It means the problem lies in how the nervous system interprets signals, not in visible tissue damage.
Modern pain science recognizes fibromyalgia as a legitimate neurological condition involving altered pain modulation. Unfortunately, outdated views still lead some healthcare providers to rely too heavily on test results, overlooking the lived reality of patients.
Education—both for patients and professionals—is key to changing this narrative.
Approaching Chest Pain in Fibromyalgia More Effectively
When chest pain is driven primarily by nervous system hypersensitivity, treatment focused solely on inflammation is unlikely to help. More effective approaches often include:
-
Gentle movement and breathing exercises
-
Nervous system regulation techniques
-
Stress management and pacing
-
Physical therapy focused on desensitization
-
Sleep optimization
-
Psychological support when fear and anxiety are prominent
The goal is not to “push through” pain, but to calm an overloaded system and gradually rebuild tolerance.
Every person’s experience is different, and management should be individualized, compassionate, and flexible.
Living With Unpredictable Pain: The Emotional Side of Fibromyalgia
Fibromyalgia does not only affect the body—it affects identity, confidence, and daily decision-making. Chest pain, in particular, can make people feel unsafe in their own bodies.
Understanding that this pain does not always signal damage or danger can be profoundly relieving. Knowledge reduces fear, and reduced fear often leads to less pain over time.
Validation matters. Being believed matters. And recognizing fibromyalgia as a condition that can affect the chest—without inflammation—helps people feel less alone and more empowered.
Final Thoughts: Recognizing What the Body Is Really Expressing
Not all chest pain in fibromyalgia is costochondritis. And not all costochondritis explains persistent, fluctuating symptoms. Often, what the body is expressing is an overloaded nervous system, reacting strongly to normal sensations.
Recognizing this difference prevents unnecessary treatments, reduces fear, and opens the door to more appropriate support strategies. Most importantly, it validates the experience of those living with fibromyalgia—acknowledging that their pain is real, complex, and deserving of understanding.
Awareness is not just about diagnosis. It is about respect, empathy, and better care.