For many people living with chronic pain, there’s a quiet frustration that’s hard to explain to anyone who hasn’t experienced it themselves. You take your medication exactly as prescribed. You wait. You hope. And yet, the pain remains—sometimes unchanged, sometimes only slightly dulled, but never truly gone.
If you’ve ever asked yourself, “Why don’t pain medications work for me?” or wondered whether anyone else feels the same way, the answer is yes—you’re far from alone. This experience is common among people with chronic pain conditions, nerve pain, autoimmune disorders, and long-term inflammatory illnesses.
In this article, we’ll explore why pain meds sometimes barely touch the pain, the science behind medication resistance, emotional and psychological factors, and what options may help when standard treatments fall short.
Understanding Chronic Pain vs. Acute Pain
One of the biggest reasons pain medication doesn’t work as expected is because not all pain is the same.
Acute pain—like a broken bone, surgery recovery, or a burn—usually responds well to traditional painkillers. These medications were designed with short-term pain in mind.
Chronic pain, however, is different.
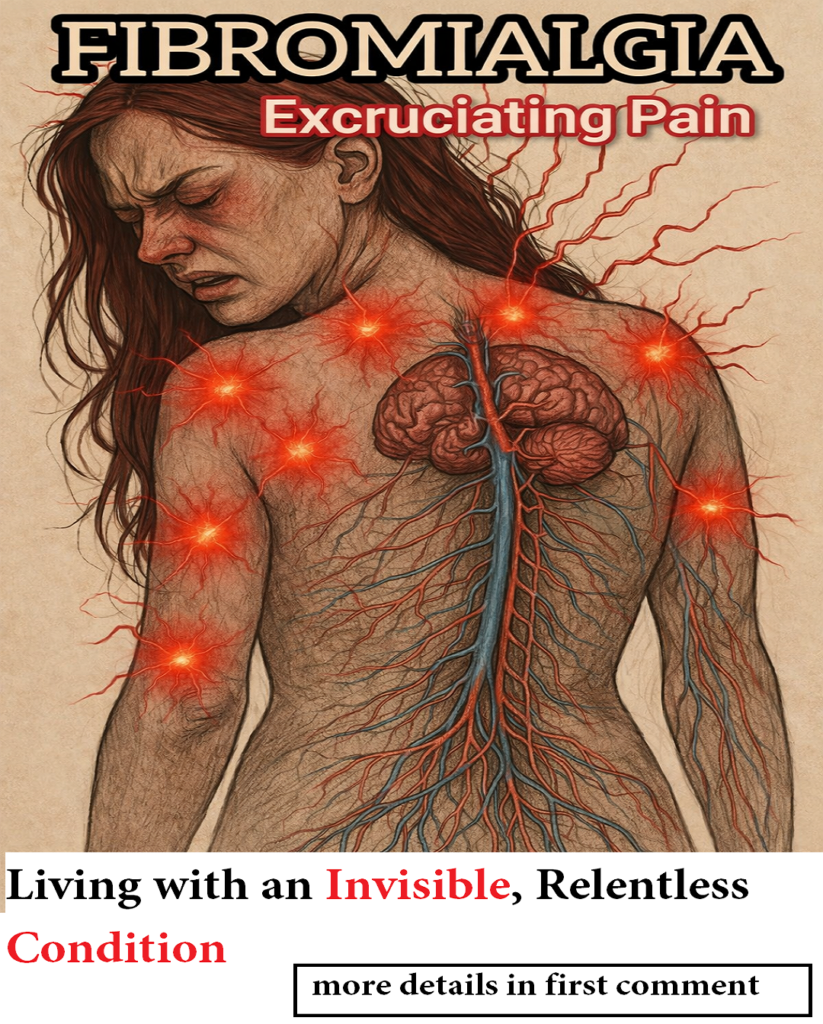
Chronic pain lasts for months or even years and often continues long after the original injury has healed. Conditions such as fibromyalgia, arthritis, migraines, neuropathy, and chronic back pain involve complex changes in how the nervous system processes pain signals.
Because of this, medications that work for acute pain often feel ineffective—or barely noticeable—for chronic pain sufferers.
“I Took the Medication… So Why Does It Still Hurt?”
This is one of the most searched questions related to pain management, and it highlights a painful reality: pain medication doesn’t always address the root cause.
Here’s why that happens:
-
Pain signals may be amplified by the nervous system
-
The brain may become hypersensitive to pain over time
-
Inflammation may be ongoing, not temporary
-
Nerve damage may not respond to standard analgesics
In many cases, the medication is doing something—but the pain is so intense or complex that the relief feels insignificant.
When Pain Meds Stop Working Over Time
Another common issue is medication tolerance.
When pain medications are used regularly, the body can adapt. Over time, the same dose that once helped may no longer provide relief. This is especially common with:
-
Opioid painkillers
-
Certain nerve pain medications
-
Muscle relaxants
-
Long-term NSAID use
Tolerance doesn’t mean the pain is “worse” because you’re weak. It means your nervous system has adjusted, requiring different strategies to manage pain effectively.
Nerve Pain and Why It’s So Hard to Treat
Many people who say pain meds barely touch their pain are dealing with neuropathic pain.
Nerve pain feels different from other types of pain. It’s often described as:
-
Burning
-
Stabbing
-
Electric shocks
-
Tingling or numbness
-
Deep aching that won’t fade
Traditional painkillers like acetaminophen or ibuprofen often don’t work well for nerve pain because the problem isn’t inflammation or injury—it’s faulty nerve signaling.
This explains why someone can take pain medication and still feel like their pain is untouched.
Chronic Illness and Invisible Pain
Living with a chronic illness adds another layer of complexity.
Autoimmune diseases, connective tissue disorders, and chronic fatigue conditions often involve systemic pain, meaning the pain isn’t coming from one clear source. Instead, it’s widespread, unpredictable, and exhausting.
This kind of pain can fluctuate daily, making it hard to medicate consistently. On some days, pain meds may offer mild relief. On others, they may feel useless.
This unpredictability is emotionally draining and can leave people feeling hopeless or misunderstood.
The Emotional Side of Pain Medication Failure
Pain isn’t just physical—it’s deeply emotional.
When medication doesn’t work, it can lead to:
-
Frustration
-
Anger
-
Anxiety
-
Depression
-
Feelings of helplessness
Many people begin to question themselves:
“Am I exaggerating?”
“Why does nothing help me?”
“Will I feel like this forever?”
These thoughts are incredibly common, yet rarely spoken out loud. The emotional toll of unmanaged pain can be just as heavy as the physical discomfort.
Central Sensitization: When the Brain Amplifies Pain
One of the most important concepts in chronic pain science is central sensitization.
This occurs when the brain and spinal cord become overly sensitive, amplifying pain signals even when there’s no new injury. Essentially, the nervous system stays in “high alert” mode.
In these cases, pain medications may dull symptoms slightly, but they don’t reset the nervous system—which is why relief feels minimal or temporary.
This is often seen in conditions like:
-
Fibromyalgia
-
Chronic migraine
-
Irritable bowel syndrome
-
Chronic pelvic pain
Understanding this can be validating. It explains why the pain feels real, intense, and resistant to treatment.
Why Doctors Sometimes Struggle to Help
Many patients feel dismissed when they say pain meds don’t work. This usually isn’t because doctors don’t care—but because chronic pain is notoriously difficult to treat.
Medical training historically focused on acute pain, not long-term pain conditions. As a result, treatment plans may rely too heavily on medication alone, without addressing lifestyle, nervous system regulation, or mental health support.
This gap leaves many patients feeling unheard.
Are Stronger Pain Meds the Answer?
It’s natural to think that stronger medication might finally bring relief. However, stronger painkillers don’t always mean better pain control—especially for chronic pain.
In some cases, higher doses can actually:
-
Increase pain sensitivity
-
Cause rebound pain
-
Lead to dependence or side effects
-
Worsen fatigue and brain fog
That’s why many pain specialists now recommend multimodal pain management instead of relying on medication alone.
Alternative Approaches When Pain Meds Aren’t Enough
When pain medication barely touches the pain, combining approaches often works better.
Some commonly recommended strategies include:
-
Physical therapy tailored to chronic pain
-
Gentle movement like stretching or swimming
-
Cognitive behavioral therapy for pain
-
Mind-body techniques such as meditation or breathwork
-
Heat or cold therapy
-
Sleep optimization
These approaches don’t “cure” pain, but they can reduce its intensity and improve daily functioning over time.
The Importance of Being Believed
One of the hardest parts of chronic pain is not being believed—especially when medication doesn’t provide visible relief.
Pain is subjective. There is no single test that measures how much someone hurts. If pain meds don’t work for you, it does not mean your pain isn’t real.
Validation matters. Being heard matters. And advocating for yourself can make a difference in finding better care.
What You Can Say to Your Doctor
If you feel like pain meds barely touch your pain, it may help to be specific when speaking with your healthcare provider.
Instead of saying:
“The meds don’t work.”
Try saying:
“The medication reduces my pain slightly, but I’m still unable to function normally.”
This opens the door to a broader discussion about alternative treatments and long-term strategies.
You Are Not Failing at Pain Management
Pain that doesn’t respond to medication can make people feel like they’re doing something wrong. They aren’t.
Chronic pain is complex, layered, and deeply personal. What works for one person may not work for another. Needing different solutions is not a weakness—it’s a reality of long-term pain conditions.
Final Thoughts: You’re Not Alone in This
If you’ve ever wondered whether anyone else feels like pain meds barely touch their pain, the answer is a resounding yes. Millions of people live with pain that doesn’t respond well to standard treatments.
While that reality is frustrating, it’s also a reminder that your experience is valid—and shared by many others walking the same path.
Relief may not always come from a single pill, but with the right support, understanding, and combination of strategies, life can still hold moments of comfort, control, and hope.