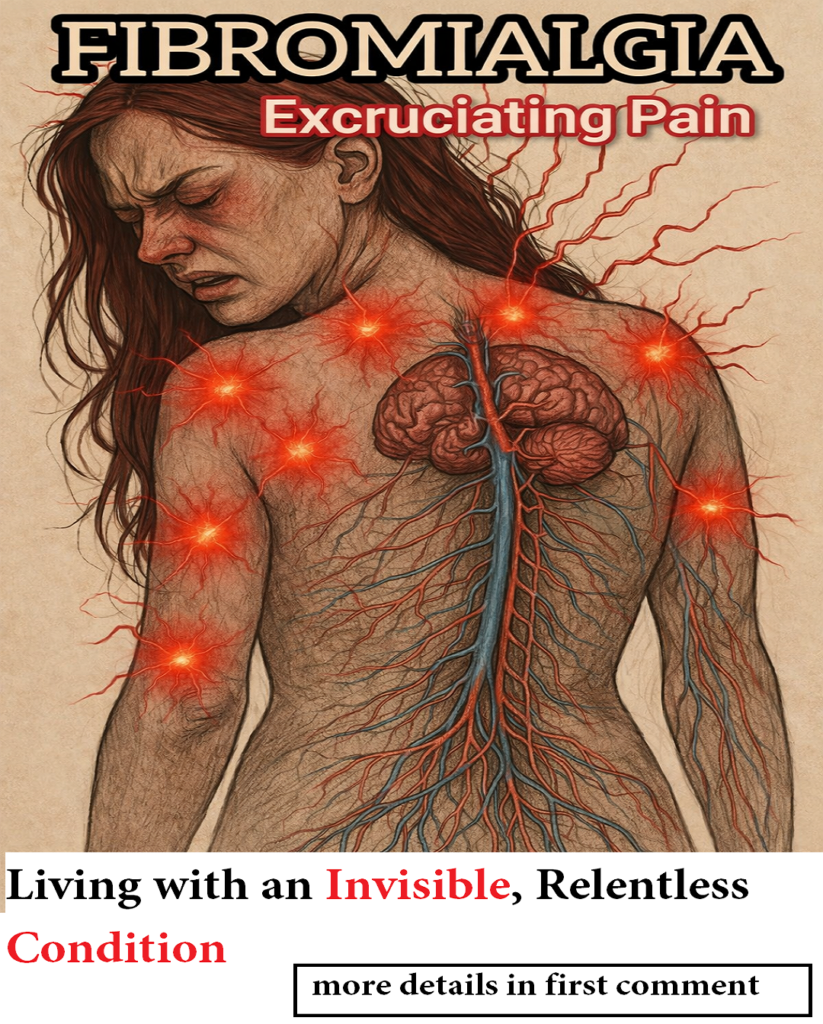
Many people living with fibromyalgia struggle to describe their pain. One of the most common phrases you will hear is, “It feels like my bones hurt.” The pain is deep, persistent, and difficult to pinpoint, leading many to believe that the problem lies within the bones themselves.
However, fibromyalgia is not a bone disease. There is no bone damage, erosion, or degeneration involved. Instead, fibromyalgia is a disorder of the central nervous system, where the brain and spinal cord process pain signals in an altered and amplified way.
Understanding why fibromyalgia pain feels so deep — and why it is often mistaken for bone pain — is essential for reducing stigma, improving diagnosis, and helping patients feel validated.
This article explores why fibromyalgia pain feels like it comes from inside the bones, how the nervous system creates this sensation, and why normal medical tests do not mean the pain is imagined.
Understanding Fibromyalgia: A Neurological Pain Disorder
Fibromyalgia is a chronic pain condition characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties often referred to as fibro fog. Unlike inflammatory or degenerative diseases, fibromyalgia does not damage tissues in a way that appears on imaging scans.
Instead, the condition is rooted in central sensitization, a process where the nervous system becomes overly responsive to sensory input. Signals that would normally be harmless — such as light pressure, posture changes, or mild muscle tension — are interpreted by the brain as painful.
This altered pain processing causes pain to feel:
-
Constant and diffuse
-
Deep and penetrating
-
Difficult to localize
-
Disproportionate to physical findings
Because the pain does not remain on the surface of the body, many people perceive it as coming from deep inside, often describing it as bone pain.
Why Fibromyalgia Pain Feels Like It’s in the Bones
The sensation of pain “inside the bones” is one of the most misunderstood aspects of fibromyalgia. This feeling does not mean that the bones are affected. Instead, it reflects how the brain interprets pain coming from multiple deep tissues at once.
Fibromyalgia primarily affects:
-
Muscles
-
Tendons
-
Ligaments
-
Fascia (connective tissue)
-
Joints
These structures are rich in nerve endings and play a constant role in movement, posture, and balance. When pain signals from these areas are amplified by the nervous system, the brain struggles to identify a single source.
As a result, pain is perceived as:
-
Coming from within the body
-
Spread across large areas
-
Deep rather than superficial
This explains why many patients say things like:
-
“It feels like my whole body is injured from the inside.”
-
“It’s like my bones are aching all the time.”
The pain is real, but its origin is neurological, not structural.
Characteristics of Fibromyalgia “Bone-Like” Pain
Although fibromyalgia pain varies from person to person, there are common features that distinguish it from other types of pain.
Widespread and Symmetrical Pain
Fibromyalgia pain usually affects both sides of the body and multiple regions at once. Unlike localized injuries, it does not stay confined to one joint or muscle.
Commonly affected areas include:
-
Neck and shoulders
-
Upper and lower back
-
Hips and thighs
-
Arms and legs
This widespread pattern reinforces the feeling that pain is coming from deep inside the body.
Different Pain Sensations at Different Times
People with fibromyalgia describe their pain using many words, including:
-
Burning
-
Pressing
-
Squeezing
-
Throbbing
-
Stabbing
-
Aching
Some days, the pain feels like extreme stiffness and heaviness. On others, it may feel sharp or electric. These changing sensations are a hallmark of nervous system involvement.
Stiffness, Weight, and Soreness
Morning stiffness is common in fibromyalgia, making the body feel rigid and sore upon waking. Many patients describe a sensation of carrying extra weight inside their body, even when no swelling is present.
This contributes to the belief that the pain is skeletal in origin, when it is actually related to muscle tension and altered pain perception.
Pain Triggered by External Factors
Fibromyalgia pain is often worsened by:
-
Cold or damp weather
-
Emotional or psychological stress
-
Physical exertion
-
Poor or disrupted sleep
These triggers directly affect the nervous system, further confirming that fibromyalgia is a neuro-sensory condition rather than a structural one.
Why X-Rays, CT Scans, and MRIs Are Normal
One of the most frustrating experiences for people with fibromyalgia is being told that all tests are normal.
Bone scans, X-rays, and CT scans typically show:
-
No fractures
-
No degeneration
-
No inflammation
-
No visible abnormalities
This often leads to misunderstanding by healthcare providers, family members, and even patients themselves.
However, normal imaging does not invalidate fibromyalgia pain. Instead, it confirms that the pain is caused by how the nervous system processes signals, not by visible tissue damage.
Pain does not always require a detectable injury to exist.
Central Sensitization: The Root of Fibromyalgia Pain
Central sensitization is the process that explains why fibromyalgia pain feels intense, constant, and deep.
In this state:
-
The nervous system stays in “high alert” mode
-
Pain pathways become overactive
-
The brain amplifies sensory input
Signals that would normally register as pressure, movement, or mild discomfort are interpreted as pain. Over time, the nervous system learns this pattern, making pain persistent even in the absence of injury.
This explains why fibromyalgia pain:
-
Persists for years
-
Moves from place to place
-
Feels disproportionate
-
Is resistant to traditional painkillers
Fibromyalgia Is Not “All in the Head”
A common and harmful myth is that fibromyalgia pain is psychological. While emotions and stress can influence symptoms, fibromyalgia is not imaginary.
Scientific research shows measurable differences in:
-
Brain activity
-
Neurotransmitter levels
-
Pain signal processing
The pain is neurological, not imagined — and not under voluntary control.
Dismissing fibromyalgia pain causes additional suffering, delays treatment, and increases emotional distress.
How Fibromyalgia Affects Daily Life Beyond Pain
Although pain is the most visible symptom, fibromyalgia affects many aspects of life.
People often experience:
-
Chronic fatigue
-
Non-restorative sleep
-
Memory and concentration difficulties
-
Sensory sensitivity
-
Emotional exhaustion
Fibromyalgia may not damage bones, but it erodes comfort, energy, sleep quality, and overall well-being.
Living with constant pain requires daily adaptation, pacing, and self-management — often without external validation.
Why Language Matters When Describing Fibromyalgia Pain
When people say “my bones hurt,” they are not being inaccurate — they are trying to express the depth and severity of their pain using familiar language.
Instead of correcting patients harshly, it is more helpful to explain:
-
What the pain sensation means
-
Why it feels deep
-
How the nervous system is involved
Validating the experience while educating about the cause builds trust and understanding.
Final Thoughts: Real Pain Without Visible Damage
Fibromyalgia pain is real, intense, and life-altering, even though it does not appear on scans or tests.
It does not break bones, but it disrupts:
-
Sleep
-
Movement
-
Energy
-
Emotional balance
Understanding that fibromyalgia pain comes from altered nervous system processing — not bone damage — helps reduce stigma and promote compassionate care.
Pain does not need to be visible to be real.
And fibromyalgia pain, though invisible, is deeply felt.