For many people living with fibromyalgia, pain is not evenly distributed across the body. While widespread pain is a defining feature of the condition, the legs—particularly the thighs—often become one of the most disabling and life-altering areas. The pain here is not just uncomfortable; it can be intense, persistent, and deeply exhausting, interfering with the most basic movements of daily life.
Walking short distances, standing in one place, climbing stairs, or even sitting for too long can feel overwhelming. Many describe their thighs as feeling heavy, burning, stiff, weak, or painfully sensitive, as if the muscles are constantly overworked despite minimal activity. Understanding why fibromyalgia affects the thighs so severely is essential for recognizing the true impact of this condition—and for responding with empathy rather than judgment.
Understanding Fibromyalgia and Chronic Leg Pain
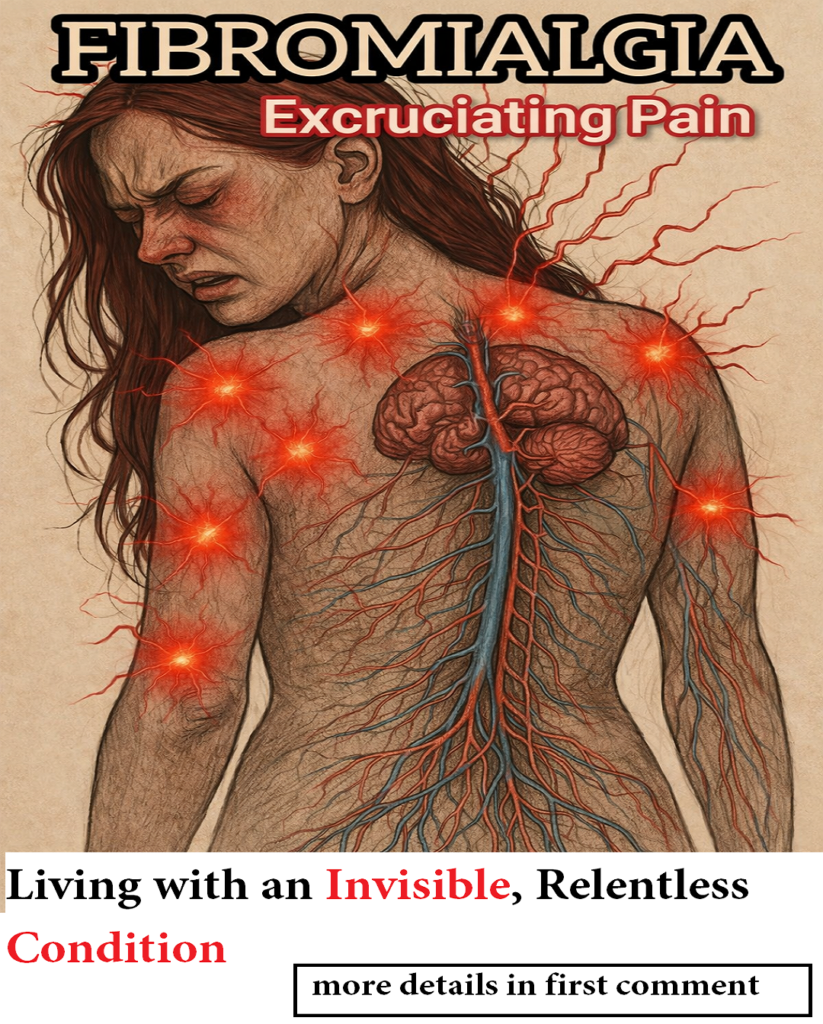
Fibromyalgia is a chronic neurological condition characterized by central sensitization, a process in which the brain and spinal cord amplify pain signals. Unlike injuries or inflammatory disorders, fibromyalgia pain does not usually stem from visible tissue damage. Instead, the nervous system itself becomes hypersensitive, interpreting normal sensory input as painful.
This explains why fibromyalgia leg pain, especially in large muscle groups like the thighs, can feel severe even when medical tests show no abnormalities. The pain is real, but its source lies in how the nervous system processes signals—not in muscle tears, arthritis, or structural damage.
Because the thighs are heavily involved in posture, balance, walking, and weight-bearing, they are constantly sending sensory information to the brain. In fibromyalgia, that constant communication becomes distorted, turning everyday movement into a continuous pain loop.
Why the Thighs Are a Common Pain Hotspot in Fibromyalgia
The thighs contain some of the largest and most powerful muscles in the body, including the quadriceps and hamstrings. These muscles are essential for almost every basic movement—standing up, sitting down, walking, climbing, and stabilizing the body.
In people with fibromyalgia, these muscles often exist in a state of persistent tension. The nervous system continuously signals danger, even when no actual harm is present. Over time, this leads to:
-
Constant muscle tightness
-
Reduced oxygen delivery to tissues
-
Increased sensitivity to pressure
-
Rapid onset of muscle fatigue
As a result, the thighs may feel sore and exhausted even after minimal effort. Many people describe the sensation as if they have completed intense physical exercise—despite doing very little.
Types of Thigh Pain Common in Fibromyalgia
Fibromyalgia thigh pain is not one-dimensional. It can present in different ways, sometimes changing throughout the day or worsening after activity.
Deep, Aching Muscle Pain
This pain often feels like it comes from deep within the muscles, rather than the skin or joints. It may be constant and difficult to ignore.
Burning or Stinging Sensations
Some people experience nerve-like pain, described as burning, prickling, or electric sensations in the thighs.
Stiffness and Reduced Mobility
Morning stiffness or stiffness after resting is common, making it hard to start moving again.
Weakness and Instability
Many people feel as though their legs might “give out,” even if muscle strength tests appear normal.
Heaviness or Weighted Sensation
A feeling that the legs are unusually heavy, slow, or difficult to lift is frequently reported.
These sensations can fluctuate, often worsening in the evening or after seemingly small activities.
The Role of the Central Nervous System in Fibromyalgia Leg Pain
One of the most important factors in fibromyalgia thigh pain is central nervous system hypersensitivity. The brain and spinal cord misinterpret normal muscle signals as threats, amplifying pain responses far beyond what the body is actually experiencing.
This leads to a constant state of alert, where muscles are treated as if they are injured—even when they are not. Over time, this process can cause:
-
Increased pain perception
-
Muscle guarding and tension
-
Reduced pain tolerance
-
Heightened response to pressure or movement
In large muscle groups like the thighs, this effect is magnified due to their constant use. The brain perceives these muscles as perpetually overloaded, creating a cycle of pain, tension, and fatigue.
Circulation and Autonomic Nervous System Changes
Fibromyalgia is also associated with dysregulation of the autonomic nervous system, which controls automatic body functions such as circulation, temperature regulation, and muscle recovery.
This dysfunction may contribute to symptoms like:
-
Poor blood flow to the legs
-
Tingling or numbness
-
Sensitivity to cold or heat
-
Slow recovery after mild activity
-
Swelling or a sensation of pressure
These circulation-related issues can make thigh pain worse as the day progresses. Many people notice that their legs feel heavier and more painful in the evening, even if they have not done anything strenuous.
Chronic Fatigue and Non-Restorative Sleep
Another major contributor to fibromyalgia thigh pain is chronic fatigue syndrome–like exhaustion and poor sleep quality. Fibromyalgia is well known for non-restorative sleep, meaning the body does not properly recover overnight.
When muscles do not get adequate rest, they remain in a state of fatigue. This explains why many people wake up with:
-
Sore, stiff thighs
-
Weak or shaky legs
-
Difficulty standing or walking in the morning
Instead of starting the day refreshed, the body begins already depleted. This constant lack of recovery compounds pain and reduces physical resilience over time.
Fear of Movement and Loss of Confidence
The combination of pain, weakness, stiffness, and fatigue often leads to fear of movement. Many people with fibromyalgia worry about falling, losing balance, or not being able to complete tasks once they start.
This fear is not irrational. When your legs feel unreliable, every step requires mental effort. Over time, this can result in:
-
Reduced physical activity
-
Increased muscle deconditioning
-
Heightened pain sensitivity
-
Emotional distress and frustration
It is important to emphasize that this is not laziness or lack of motivation. It is the result of a nervous system under constant strain, trying to protect the body from perceived danger.
How Fibromyalgia Thigh Pain Affects Daily Life
When the thighs are affected, mobility becomes limited, and daily routines must be adapted. Simple activities such as grocery shopping, household chores, or standing in line can become exhausting challenges.
Loss of independence is one of the most emotionally difficult aspects of fibromyalgia. When the legs fail to cooperate, people may feel embarrassed, misunderstood, or dismissed—especially when others cannot see the pain.
Recognizing the severity of fibromyalgia thigh pain is essential for creating supportive environments at home, work, and in healthcare settings.
Living With Fibromyalgia Thigh Pain: Compassion Matters
Fibromyalgia thigh pain is real, deep, and disabling. It affects not just the body, but also confidence, independence, and emotional well-being. Understanding its neurological basis helps dismantle harmful myths that dismiss the condition as exaggerated or psychological.
When the legs are compromised, life must be adjusted—and that adjustment deserves respect. Empathy, patience, and proper support can make a meaningful difference for those living with fibromyalgia every day.
Pain that cannot be seen is still pain. And leg pain that limits movement reshapes an entire life.